*In the beginning of the pandemic, I was asked by a healthcare system to write a piece helping healthcare workers and their loved ones with the trauma of Covid 19. In the past two years I have had the privilege of working in health systems with passionate, dedicated, and truly exhausted healthcare providers—and it seems that it’s important to once again help this group of people with the recovery and repair necessary as we go through this stage of the pandemic—as it shifts to being a chronic stressor. This is a follow up to that first piece. It is longer than my typical blog pieces because it is meant to be a comprehensive resource for people who need the information all in one place. Please share in any network you think would be helpful.
I am aware that I am writing this piece as Florida begins to assess the damage from Hurricane Ian—and there is such a contrast between the trauma inflicted by a massive natural disaster—where the wreckage is obvious—and the repeated trauma of Covid where the wreckage may not be as visible. This seems to be true for many of the leaders I am working with, but especially true for the healthcare providers I am working with. They can’t see the wreckage so they feel lost or disoriented or confused by why they feel so exhausted or burned out.
The job a healthcare provider was never easy. Much of healthcare work is a form of chronic or sustained trauma. Trauma in the everyday world is seen as something extraordinary—and any reaction to it is often seen as a problem---you have acute trauma disorder, or Post-Traumatic Stress Disorder. But there are professions—medicine, first responders, military, social work, psychology, and education—to name a few—where there is a high level of sustained and repeated trauma. Where trauma and exposure to trauma are baked into the job. Where rather than a disorder, you engage in what should actually be called functional. So rather than post-traumatic stress disorder, you actually live with a “Functional Repeated Trauma System” –where you create a system of managing the ongoing retreated trauma and vicarious trauma and learn to maintain a balance of responsiveness and protectiveness. This dynamic system is designed to allow you to adjust and adapt to the ongoing sustain stressor of trauma. It’s not dysfunctional or a disorder—it’s an adaptive dynamic system.
But it’s a system that was overloaded during the pandemic. Throughout your whole careers, you worked long hours and you have endured terrible losses of patients. You had years of grueling training. You had to learn how to manage fear, grief and shame the best ways you knew how—mostly by compartmentalizing—a strategy research showed didn’t work that well in the best of times.[i] But the scale of Covid-19 was different. You were seeing patients who need 8 blood transfusions. You were seeing young, previously healthy people stroke out. You were having to hold the phone to the ear of dying patients and shepherd families though loss. You had to endure a new level of animosity and rudeness from families and distrust of medicine and science. Your work, which has always been stressful, became war-level traumatic and it is really important that all health professionals, the people who love them, and the people who run the health systems understand the impact of this increase in trauma and take seriously the kind support that is needed to plan the support that will be necessary through this recovery.
The level of trauma that occurred during the pandemic was dangerous, with an increase in physician suicide, and more recently, with an marked increase in physician burnout and a decrease in job satisfaction and work/life balance. What is crucial to understand is that it isn’t a lack of capacity to manage trauma, but an imbalance in the amount of trauma and the capacity for, and attention to, recovery for both individuals and systems.
Physiological and Psychological Impact of Trauma
I want to start first with the physiological and psychological impact of trauma. These things aren’t separate—because trauma elicits an emergency response system from our bodies and our brains are part of our physiology—not some separate aspect. Trauma responses are normal and not some sign of psychological weakness. A working definition of trauma is any event that overwhelms your system of protections and leaves you fearful of your life and/or safety rendering you helpless. This is where Covid-19 is different than many crises that healthcare providers and the healthcare systems have grappled with before—typically you haven’t had to fear for your own safety as you have cared for patients—and you haven’t feared for the safety of your family as you have cared for patients. And your families haven’t had to worry about your safety or protect themselves from you. And healthcare leaders haven’t had to try to support their people from a distance and worry about the safety of their people or their loved ones all while managing their job.
When I talk about trauma it is important to understand that all trauma is not equal. If the hospital you were working in was affected by a single incident trauma—if it were hit by an earthquake, for example, it would be horrible and traumatic. You would have all the impact of severe stress which overwhelms the normal system of psychological defenses and floods your body with adrenaline. In short term trauma, the system is overwhelmed, and the effect is an over-sensitized system. This adrenaline helps us focus in a crisis and this ‘hypervigilance’ is often trained into professionals as a requirement of their job in roles like Emergency Room doctors, police, first responders and military. The definition of hypervigilance is “let me pay attention to every sight sound and other sensory input available to increase my awareness of the environment and thus lower my chances of being victimized by an unknown.[ii]” Other symptoms of a one-time trauma are startle response, flashbacks, nightmares, difficulty eating, difficulty sleeping, difficulty concentrating, or persistent avoidance of anything that reminds the person of the traumatic event. You may recognize some of these symptoms right now. They are common and they are a pretty normal response to trauma. If these symptoms persist for a month, they meet the criteria for PTSD.[iii]
But what the healthcare world is experiencing right now is the equivalent of getting hit by an earthquake every day. A single incident of trauma catches us off guard and breaks through our defenses. But when trauma is repeated we don’t wait to get ‘caught off guard’ -- we unconsciously, yet wisely, build a system of defenses against being overwhelmed and getting caught off-guard again. Building defenses to survive and experience the repeated trauma conserves our energy for survival. Instead of getting flooded with emotion—with terror, fear, and all the responses to it—we go numb, we feel nothing, and we do whatever we have to in order to maintain our distance from ourselves and others. Repeated trauma is really three forms of trauma: What is happening (the massive scale of illness and death), the psychological protections you are using to survive the trauma, and what isn’t happening: all the aspects of your life that have needed to halt because of the trauma that is happening. And healing from repeated trauma will need to address all three.[iv]
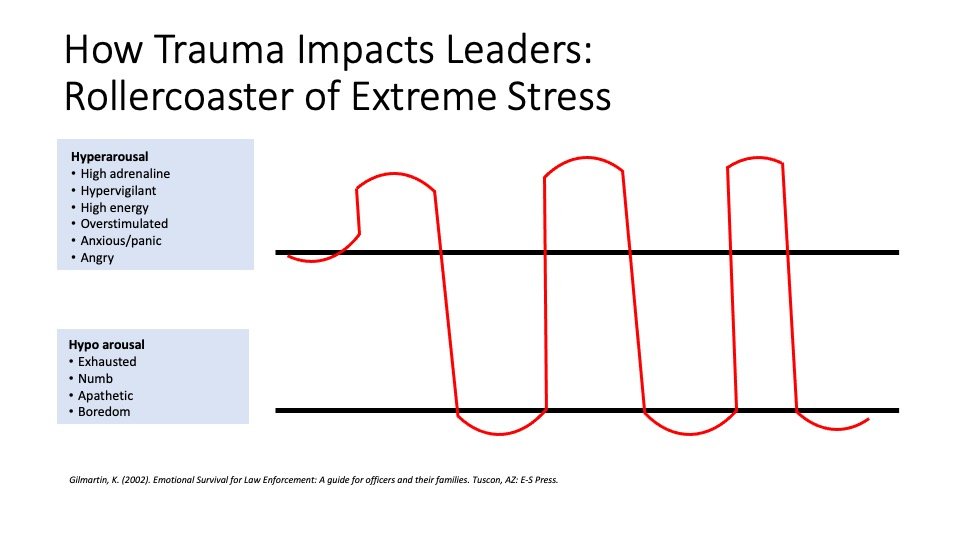
There is a way that the healthcare world has always had a relationship with repeated trauma—a way to balance survival skills with growth capacity. But the constant pressure of Covid disrupted the balance and shifted the ‘functional repeated trauma system’ into survival mode. This survival mode has you toggling back and forth between a traumatic workplace and going back to your families—so that you are experiencing a roller coaster of trauma responses from high adrenaline, hypervigilance and energy to exhausted, shut down, apathetic and angry.
As healthcare folks you learn about the impact of stress on the body but you are enculturated to believe that you are immune from this response. You aren’t. Yes, you trained long hours and you can shift your attention from your bodies, but your physiology is having an experience, and you will be affected by it. This roller coaster you are experiencing is real and it is important to own the impact of the rollercoaster on your brain and body. Understanding this will help you survive the trauma while it is happening with greater resilience, and it will help you understand the impact of the trauma when you are finally able to heal from it. To understand it better look at the following illustration.
When you are on-shift, you are on the top of this illustration—you are hit with a flood of adrenaline— you are in a necessary state of hypervigilance—paying attention, highly energized, ready for action. And when you go off shift you are below the lines-- your body sinks into a state that may be exhausted, apathetic, and irritable.[v] As Gilmartin, who works with police professionals states, “for every action there is an equal and opposite reaction,” and this rollercoaster is your body’s attempt to recover from the onslaught of stress hormones. This recovery typically takes 18-24 hours making it likely that on most days you will barely get the time to recover before you are back in it. You may notice that you feel more ‘alive’ at work. That you feel more like ‘yourself’ with the adrenaline and you feel more detached or numb when you are home. This crash in to numb may make it harder to connect to your families or friends when you are home, or make it harder to connect with them via phone or FaceTime if you have moved away to protect them. Trauma makes it seem like the only people we can connect with are people who are in the trauma with us. It’s a ‘war buddy’ phenomenon: the people we are with ‘above the line’ can feel more connected to us than the people we are with ‘below the line.’ This doesn’t mean we love them less, but this is physiological and psychological response to trauma. But it doesn’t have to rule your reality, and there are ways to manage this roller coaster and bring awareness to your recovery and reconnection to support survival in this difficult time.
What can health professionals do right now to support recovery and repair of the physiological and psychological trauma of Covid-19.
1) You have to own the roller coaster. By being aware of the impact on your body and brain you have some choices about what actions you can take to bring yourself into the best possible state.
2) Plan your transitions between work and home: create a ritual that helps you connect with people, and previous aspects of yourself (favorite music, something nourishing).
3) Avoid television, or things that make you more likely to sit in ‘numb’ for too long.
4) Attend to your body. Above the line, you want to do things that ‘soothe’ you. Below the line you want to do things that bring you back into a feeling state.
5) Start wherever you are: sometime simply stating how you feel “I feel numb” allows you to be heard and understood and help you feel more connected to yourself and others and mitigate the experience of feeling detached.
What can loved ones do right now to support recovery and repair of their health care professional’s physiological and psychological trauma of Covid-19:
1) Stay engaged: Imagine holding the other end of the rope. Sometimes you will hold it lightly, and sometimes you will tug on it. But stay connected in ways that you can.
2) You need to have conversations—even when they feel awkward and repetitive—for all of you during this time: what is helpful, what is stressful, what are your signs of stress, how will I know you need help, what are you grateful for, what brings you joy?
3) Your health professional may not be able to support you in the way you need right now, who else can be on your team to support you and your family right now? Who else can you talk to to make sure you aren’t alone with your worries either?
4) Reacquaint yourselves to the activities that brought you joy, and try to some new things as well. Be curious about what is important to you now.
What can healthcare leaders do right now to support repair and recovery of their colleagues and healthcare professional’s physiological and psychological trauma of Covid-19.
1) Help your health professionals and colleagues understand and own the impact of stress and trauma. Normalize it and encourage conversation and coping.
Make sure that the mental health resources are easily available, easy to find and widely distributed.
2) All leaders should have conversations with their teams: what is helpful, what is stressful, what are your signs of stress, how will I know you need help, what are you grateful for, what brings you joy? These are not conversations that you have just once. They are ongoing and help you stay in contact with the level of stress people are experiencing.
3) Health care leaders need to be brave enough to welcome the truth from their people in terms of what their health care providers are feeling and the level of stress. You need to thank people for the information. Information is the only way you will be able to lead effectively and they will only give it to you if you listens and don’t judge or punish.
The Hidden Wound: Moral Injury
But the problem with surviving and healing from trauma is that often the discussion stops with the physiological and psychological impact. The discussion stops at the symptoms of PTSD and never gets to the impact of repeated trauma—the changes we make in ourselves to survive, let alone one of the biggest hidden wounds of trauma: moral injury. We have a self-concept of ourselves as a person with integrity who is helpful and does the right thing. Most people never have to test this self-concept of themselves, and in trauma, this test can be brutal. It can be devastating to a health professional, whose self-concept is to save people’s lives, to watch person after person die, with no real ability to change the outcome. It doesn’t matter if realistically it wouldn’t have been possible there is something mammalian about our desire to be effective in the face of doing our jobs as helpers. Indeed, the search and rescue dogs during 9/11 got so distraught and depressed at not finding survivors that their handlers had first responders hide in the rubble to be found so the dogs didn’t’ experience their own version of moral injury. The psychiatrist Joseph Shay calls PTSD a primary injury--it's symptoms are visible like the break of a bone. But a moral injury is like internal bleeding. It is a silent killer. Soldiers often report feeling like a piece of them died during the war and others have referred to it as ‘soul murder.’
It is important to note that moral injury is not a ‘psychological disorder.’ It’s deeper than that—it hits identity, it hits values, spiritualty, it hits at your very soul. It is the ‘consequence of violating one’s conscience, even if the act was unavoidable or seemed right at the time.[vi]” As health professionals you have a set of beliefs and principles that guide your work and life, “I help save people’s lives” “I never leave a patient to die alone” “I support my coworkers” “I value my family above all” and this crisis doesn’t allow you live those principles at all times and may have you behaving in ways you could have never imagined because it was never required of you. Crucially, it is about you as an individual trying to hold the weight of a collective trauma all by yourself. As a doctor, nurse, respiratory therapist or other health worker helping a patient’s family talk to a dying patient on their Ipad is holding the devastation by yourself, but it shouldn’t be yours to hold alone.
What can Health Professionals Do Right Now:
For war veterans, having to hold their own stories of moral injury—the things that they had to do to survive—is one of the risk factors for suicide with a staggering suicide rate of 22 a day. It is imperative, and may be lifesaving, for you as health professionals to know about moral injury and know that, tragically, it is part of trauma. You will need to need to hold this concept of moral injury for yourself and you need to remind your colleagues. It is a wound that will need healing, but in the short term the most important thing you can do is to not hold your experience and your story alone. This was a world-wide collective trauma. While your individual experiences are personal to you and important to you—the trauma of this pandemic was bigger than you and you must lean on others to hold it. Start with your colleagues and fellow health care workers and share the burdens you are carrying. And then bravely begin to share your stories with your loved ones as you are able, and with the systems and communities within which you work.
What Can Health Care Leaders and Loved Ones Do Right Now:
Health care providers can’t heal without help from loved ones and health care leaders. In order to heal from moral injury health professionals will need to be able to tell their stories, and most importantly, every one of us, from loved ones, to health care leaders to community members are going to have to hold these stories with them. Holding these stories means holding the humanness of not being able to rise to every occasion. It means sitting with the grief and loss and tragedy that this pandemic has wrought. It means not being able to fix it, but instead sit with it. It is, in fact, the opposite of the behavior that we have for Veterans and now for Health Care Workers, where we thank them for the service and call them ‘heroes.’ The problem isn’t that we are grateful and consider them heroic. The problem is that their lived experience of failure and helplessness during their trauma feels so far away from the word ‘hero’ that it makes them feel alien from themselves. And this alienation is dangerous. And most importantly, it keeps them, then, from trying to tell the real story, the real trauma story, where they didn’t feel heroic, or indeed it wasn’t possible to act heroic. In our attempt to be kind, we can cruelly isolate them and that is something we need to avoid. We need to simply listen and acknowledge their sacrifices. We need to let them tell us what it was like. We need for them to not hold it alone.
All of us can make a difference and have an impact on healing. All of us can engage in the small acts of connection. All of us can check in on a colleague or a friend. In fact, in research done by the state of Oregon, the most common response to ‘what does a trauma -informed leader do?” —was ‘they would greet me with a smile. “ We need to remember that no one heals alone. That the antidote to the collective repeated trauma is community.
© 2022 Gretchen L. Schmelzer, PhD
[i] Granek et al., (2012). Nature and Impact of Grief over patient loss on oncologists personal and professional lives. Archives of Internal Medicine 172 964-966. In Ofri, D. (2013). What Doctors Feel. NY: Beacon.
[ii] Gilmartin, K. (2002). Emotional Survival for Law Enforcement: A guide for officers and their families. Tuscon, AZ: E-S Press.
[iii] American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders: Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlington, VA: American Psychiatric Association, 2013.
[iv] Schmelzer, G. (2018). Journey Through Trauma. NY: Avery.
[v] This citation is a combination of Gilmartin, K. (2002). Emotional Survival for Law Enforcement: A guide for officers and their families. Tuscon, AZ: E-S Press and Siegel, D. (2010). Mindsight. New York, NY: Bantam Books
[vi] Brock, R., & Lettini, G. (2012). Soul Repair: Recovering from Moral Injury after War. Boston: Beacon Press.